Asma-1
The Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 3 (EPR3) recommend objective measures of airflow such as forced expiratory volume in 1st second (FEV1) and peak expiratory flow (PEF) to improve the assessment of severity, control, exacerbations and response to therapy. The Vitalograph asma-1™ is a hand held device that measures FEV1 and PEF. FEV1 is the “vital sign of asthma”, as it is a more sensitive measure of airflow obstruction than PEF, and is less likely to be erroneously high. Usually three (3) blows are required and the “best test” values in the session (best PEF and best FEV1), are recorded for the session in the device history. For a good test, the time to peak flow must be 120ms (milliseconds) or less, and no cough should occur in the 1st second. The Asma-1 can store up to 600 test sessions. The device uses disposable mouth pieces and operates on two (2) AAA batteries. It is recommended that the device be regularly cleaned according to the guidelines of the user’s facility.


Expiratory mouthpiece (disposable)

COPD-6
The Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 3 (EPR3) recommend of pulmonary function as “necessary for the diagnosis of asthma because medical history and physical examination are not reliable means of excluding other diagnoses or of characterizing the status of lung impairment.” The COPD-6 is a hand held device that measures forced expiratory volume in the 1st second (FEV1), forced expiratory volume in 6 seconds (FEV6), and FEV1/FEV6 ratio. The patient’s physical data (i.e., age, height, weight, gender and population group) are entered into the Vitalograph copd-6™ in order to calculate predicted values which provide a measure of comparison to values of people with similar characteristics. If a test is less than 6 seconds duration or has an abrupt end the FEV1/FVC ratio IS NOT VALID. The FEV1/FEV6 value will appear as a decimal. It is IMPORTANT to disregard the percentage value (% predicted results) below the decimal. Use the decimal value for clinical purposes related to FEV1/FEV6. Low FEV1 indicates current obstruction (impairment domain) and risk for future exacerbation (risk domain). For children, FEV1/FEV6 appears to be a more sensitive measure of severity in the impairment domain. The Vitalograph copd-6™ stores the last test session, uses the same disposable mouth pieces as the Vitalograph asma-1™ and operates on two (2) AAA batteries. It is recommended that the device be regularly cleaned according to the guidelines of the user’s
facility.
In-check Dial
The In-Check Dial is a useful tool to assess and coach inhalation technique. The DIAL simulate the resistance of different inhaler devices (metered dose inhalers and dry powder inhalers [Turbuhaler®, Diskus®]) to train persons to use more or less inspiratory force to achieve an optimal flow rate with a particular device. Proper inhalation technique is critical to assure inhaled medication is deposited in the lungs. The dial has to be set to the appropriate inhaler type being used by the person. Install the one-way filter (arrow pointing toward the person). Hold the instrument vertically with the mouthpiece uppermost, so that the rounded end of the meter can be tapped against the other hand or a horizontal surface, such as a table. A hard tap will dislodge the magnetic resetting weight, which will return the red cursor to a start position. When this has happened, turn the In-Check Dial vertically so that the magnetic weight can return to its resting position near the mouthpiece. It is important to reset the device before each inhalation attempt. Be sure the person doesn’t blow but inhales as they would in taking their inhaler medication. A steady inspiratory flow rate at or near the Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 3 (EPR3) recommended rate of 30 liters/minute for 3 to 5 seconds for metered dose inhalers (MDIs) and 60 liters/minute for 2-3 seconds for dry powder inhalers (DPIs) such as an Advair diskus is optimal. ARC encourages giving the person a “target time” – the amount of time in seconds it will them to fill up their lungs with new air and medicine if they are breathing at the right speed, based on their lung volume (FEV1). There are various models of the In Check Dial and are distinguishable by the color of the disk (i.e., white, blue or orange) that has various sized holes. It is recommended that the device be regularly cleaned according to the guidelines of the user’s facility.
Inspiratory Mouthpiece (disposable)


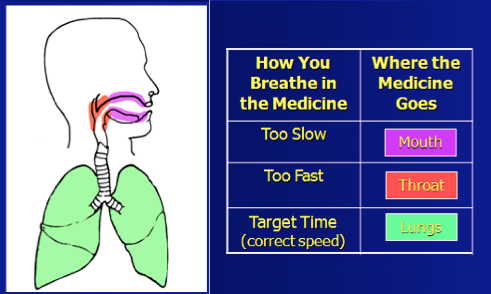
2Tone MDI Trainer
Many people with asthma do not inhale their medication properly. The 2Tone MDI Training Device helps an individual learn to inhale at the right speed. It has the shape and feel of a real inhaler but has no pressurized aerosol or medication. The 2Tone Trainer provides an audible feedback on how fast air is being inhaled. If medication is inhaled too quickly the majority is deposited in the mouth and throat rather than the lungs where it is needed. By listening to the sound the 2ToneTrainer makes, an individual can learn to adjust how they breathe in and to achieve the correct speed of inhalation. Inhaling through a 2Tone Trainer will produce one of three sounds. If no sound is produced, the person is inhaling too slowly and should speed up. If two tones are heard, the person is inhaling too fast and should slow down. The person is instructed to inhale until the 2Tone Trainer produces a single tone. Slow inhalation at a rate between 30 and 60 liters/minute increases the amount of drug reaching the lungs for maximum benefit to the individual. ARC encourages giving the person a “target time” – the amount of time in seconds it will them to fill up their lungs with new air and medicine if they are breathing at the right speed, based on their lung volume (FEV1).
Nebulizer
A nebulizer changes liquid medicine into fine droplets (in aerosol or mist form) that are inhaled through a mouthpiece or mask. Nebulizers can be used to deliver bronchodilator (airway-opening) medicines and are particularly effective in delivering asthma medications to infants and small children and to anyone who has difficulty using an asthma inhaler. Nebulizers come in home (tabletop) and portable models. Home models are powered by a compressed air machine and plug into an electrical outlet. Portable nebulizers, powered by an internal battery or cigarette lighter, are available for individuals requiring treatments away from home. When using a nebulizer, take slow, deep breaths through the mouth and if possible, hold each breath for two to three seconds before breathing out. This allows the medication to settle into the airways. A mask should be used for infants and children 5 years of age and under. Without a mask most of the intended dose will be lost; blow-by technique not effective for infants and young (EPR3, p. 251). To obtain a nebulizer, a prescription is needed from a health care provider.



Bubbles
The newly designed Bubbles the Fish Mask™ by PARI is designed for children ages 3 and older. This soft mask with its fun fish design fits comfortably on a child’s face. The front load design directs medication towards a child’s mouth. Exhalations are directed to intentionally placed vent cutouts that dramatically reduce deposition of aerosol onto your child’s face and eyes. Most efficient when used with “front-loaded” LC nebulizers, but a plastic elbow is included if for a typically less efficient “bottom-loaded” nebulizer.

Bubbles the Fish™ II
Aero Chamber
The AeroChamber® consists of a plastic tube with a mouthpiece, a valve to control mist delivery and a soft sealed end to hold the metered dose inhaler (MDI). The holding chamber assists delivery of medicine to the small airways in the lungs. This increases the medicine’s effectiveness. Its portable size, efficiency and convenience make the MDI a desirable method for inhalation treatment. The medication will be delivered into the AeroChamber®. Individuals are instructed to press the inhaler once and to breathe in slowly and deeply over 3 to 5 seconds until a full breath is taken. ARC encourages giving the person a “target time” – the amount of time in seconds it will them to fill up their lungs with new air and medicine if they are breathing at the right speed, based on their lung volume (FEV1). If the person breathes in too fast, the AeroChamber® may whistle. The person should slow down inhalation if they hear the FlowSignal® Whistle sound. Hold breath for five to ten seconds, if possible. This allows the medication time to deposit in the airways. Spacers or valved holding chambers are recommended for children and adults taking MDI medicines who have difficulty performing adequate inhalation technique (EPR3, p. 250).