Asthma Ready® Communities (ARC) is an overarching endeavor to provide standardized, evidence-based educational programs for children with asthma, families and health professionals. These programs enhance the readiness of health care professionals and facilities to provide cost-efficient care that is compliant with the Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 3. For parents and caregivers, these programs provide comprehensive steps to improve asthma control in infants and children. For facilities, Asthma Ready® is a designation indicating that the facility has participated in asthma training, has the resources and is committed to delivering appropriate services, maintaining communication standards, and conducting quality improvement efforts to ensure best practices for the care of children with asthma. Asthma Ready® is a registered federal trademark owned by the University of Missouri.
Asthma Ready® Communities (ARC) is an overarching endeavor to provide standardized, evidence-based educational programs for children with asthma, families and health professionals. These programs enhance the readiness of health care professionals and facilities to provide cost-efficient care that is compliant with the Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 3. For parents and caregivers, these programs provide comprehensive steps to improve asthma control in infants and children. For facilities, Asthma Ready® is a designation indicating that the facility has participated in asthma training, has the resources and is committed to delivering appropriate services, maintaining communication standards, and conducting quality improvement efforts to ensure best practices for the care of children with asthma. Asthma Ready® is a registered federal trademark owned by the University of Missouri.
The ARC team is located in the division of Pulmonary Medicine & Allergy, Department of Child Health, University of Missouri (MU), School of Medicine. Dr. Francisco and the clinical staff are members of University Physicians practice group, providing specialty care at MU Women’s and Children Hospital, Pediatric Specialty Clinic. Other staff represents disciplines ranging from social health science to epidemiology. The central office is located in Columbia, MO 65212
Contact Us: Info@AsthmaReady.org | Phone 573.884.8629 | FAX 573.882.6126
Address: 400 North Keene Street, Columbia, MO
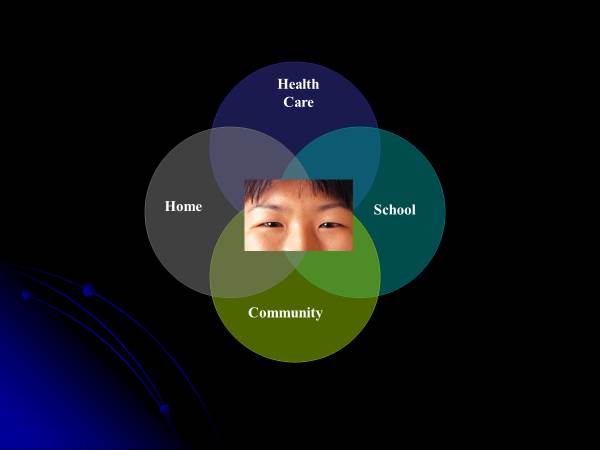
Asthma Ready® Communities uses a array of foundational principles and models to care and promote health among children and communities. Among these are: patient- and family-centered care, self-regulation, collective impact, learning health system, quality improvement, and health equity.
Patient-Centered Care
Asthma Ready® Communities values and practices patient-centered care, in which an individual’s health needs and desired health outcomes are the driving force behind all health care decisions. Patient- and family-centered care encourages a true partnership with active collaboration and shared decision making between patients, families, and providers and where the patient’s needs, values, and culture are respected. Care and communication is coordinated across health and community settings in accordance with patient and family needs and preferences for continuity and better outcomes.
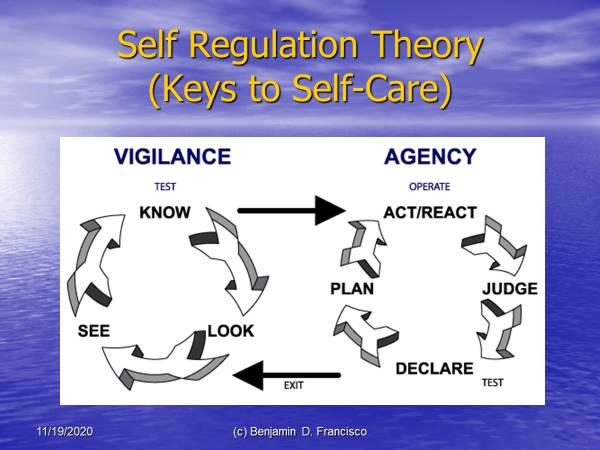
Self-Regulation / Self-Care
The process of managing and guiding one’s thoughts and feelings to engage in goal-directed actions such as organizing thoughts, behavior, feelings, controlling impulses, and solving problems constructively to improve health, well-being, and achieve goals.
Collective Impact
Collective impact is a quality improvement framework for achieving systems-level changes in communities through coordinated multi-disciplinary collaborations to address complex social issues and achieve shared goals. It is a partnership collaborative with a common agenda, shared measurements (process and result indicators), mutually reinforcing activities, open communication, and backbone agency infrastructure working together to reach goals.
Learning Health System
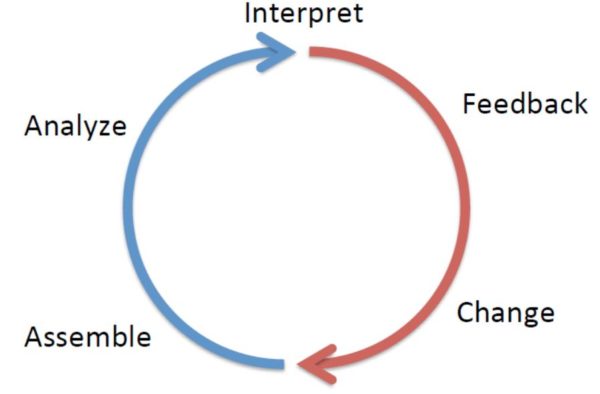
A learning health system has science, informatics, incentives, and care culture aligned for continuous improvement and innovation, with best practices embedded in the delivery process and new knowledge gleanedfrom the delivery experience to improve value, lower cost, and have better outcomes. As shown in the model, this framework has cycles common to all learning systems and three components: Afferent (blue) – gather, analyze, and interpret data; Efferent (red) – feed information into system for practice change; and scale – level of change (e.g., institution, national, or international).
Quality Improvement
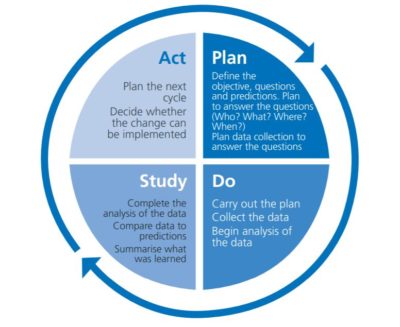
In health care, quality improvement (QI) is the framework used to systematically improve the ways care is delivered to patients. Asthma Ready Communities includes the Model for Improvement(MFI) that uses a rapid cycle process called Plan Do Study Act (PDSA) cycles to test the effects of changes. The process begins with three questions.
- What are we trying to accomplish?
- How will we know that a change is an improvement?
- What changes can we make that will result in improvement?
 Coordinated Federal Action Plan to Reduce Racial and Ethnic Asthma Disparities
Coordinated Federal Action Plan to Reduce Racial and Ethnic Asthma Disparities
The Coordinated Federal Action Plan identifies strategies for addressing barriers to implementation of The National Asthma Education and Prevention Program (National Heart Lung and Blood Institute) Expert Panel Report 3 (EPR3) guidelines-based asthma care. The strategies include: reducing barriers to guidelines-based care, increasing capacity to identify disparate communities, and delivering integrated care to children most at risk while identifying prevention best practices.These approaches when combined and applied can drastically improve asthma control for all children.