News
University of Missouri, School of Medicine ABMS Quality Improvement Award
Publications
Teaming Up for Asthma Control: EPR-3 Compliant School Program in Missouri Is Effective and Cost-Efficient
https://www.cdc.gov/pcd/issues/2017/17_0003.htm
(Approved for Publication by Journal of Asthma & Allergy Educators ) – no longer being published site host publications between 2010 and 2013
Innovative Data Analysi
Surveillanc
AAE ECI Asthma Morbidity
Using ER Data
Using Surveillance Data
MAPCP asthma data
https://health.mo.gov/living/healthcondiseases/chronic/asthma/data.php
Clinical Research
Abstracts
Adoption of Best Practices Increases Proportion of Outpatient to Acute Care Pediatric Asthma Visits
Benjamin Francisco, PhD 1; Paul Foreman, PhD 1;Sherri Homan, PhD1; Tammy Rood, DNP 1; Bhawani Mishra, PhD 2
1University of Missouri-Columbia, School of Medicine and 2University of Missouri-Columbia, Harry S. Truman Instituteof Public Policy
Rationale: Many children have uncontrolled asthma leading to frequent and costly acute care visits with notable disparities among low-income and African Americans. This 10-month intervention adapted four effective approaches (i.e., practice facilitation, collaborative learning, performance feedback, and academic detailing) known to promote implementation of expert asthma guidelines in a scalable program approved for Maintenance of Certification, Part 4 by the American Board of Medical Specialties. We hypothesized program participation would be associated with increasedadoption of best practices and correlate with both an increase in the proportion of primary care (outpatient) to acute care asthma encountersand total asthma patients in participating health centers.
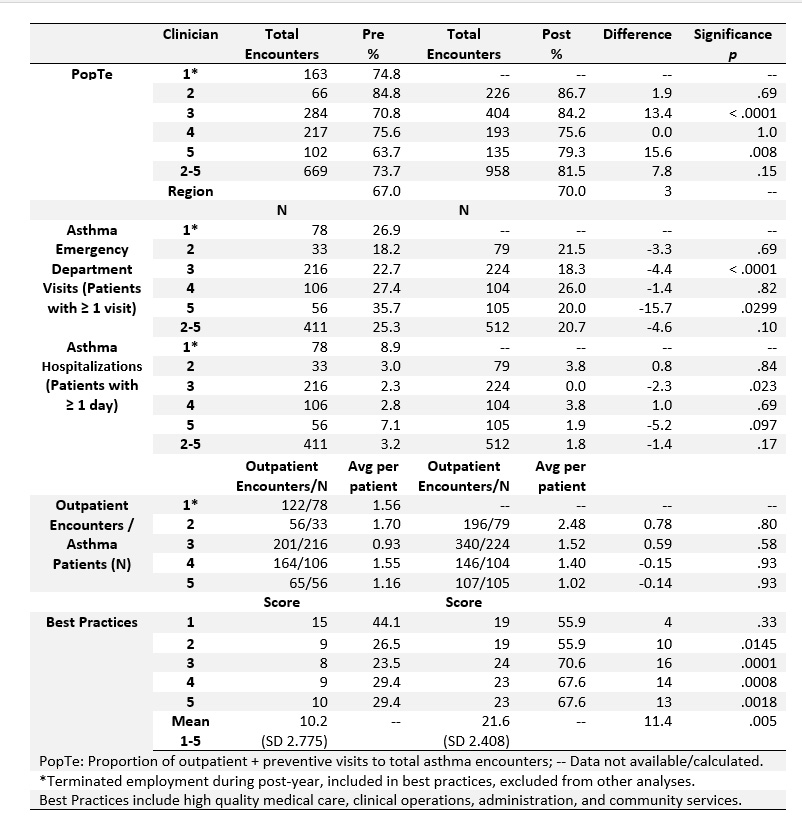
Methods:Asthma best practices (34 indicators) were surveyed before and after participation in 12 Extension for Community Health Outcomes (ECHO®) video teleconferences approved for category one CME that incorporated peer-led case studies and expert didactics. Using Medicaid administrative claims, we examined change in asthma control indicators before and at one-year intervals during and after participation. A dashboard of indicators (Asthma Risk Panel Report [ARPR]) was developed and refined with health center input to track outcomes and support care management. Regional, health center, and provider-level ARPRs were compiled and repeated over time.The primary outcome was the proportion of outpatient and preventive services to total asthma encounters (PopTe).Significance was tested using Chi-square or paired t tests.
Results:Five pediatricians participated in the intervention Asthma Care Accelerator ECHO with predominately AfricanAmerican children with asthma receiving care. Four remained at their original practice site allowing evaluation of ARPRs for a baseline year and one or more sustaining years. Across providers PopTeranged widely from 64% to 87%. There were significant increases in PopTefor two participating pediatriciansfrom 71% to 84% (p < .0001) and 64% to 79% (p = .008). Asthma emergency department visits also significantly declined for the two practices. The larger regional ARPR of >10,000 children showed a PopTe of 67% at baseline and 70% in the follow-up year.At the onset, a low rate (10 of 34 or 30%) of adoption of asthma best practices was observed. At the end of the postperiod, this rose to22 of 34 (65%). Total patients increased for three of the four participating practices.
Conclusion: This intervention has shown effectiveness in improving adoption of best practices, promoting outpatient care in lieu of acute and urgent care, andincreasing the number of children served by health centers.
Table 1. Proportion ofOutpatient to Total AsthmaEncounters, Visit Type, and Adoption of Best Practices, Pre- and Post-Intervention, Missouri Medicaid Participants (< 21 years of age)
Funding: Provided in part by the Leda J Sears Trust Fund, Health Forward Foundation, and US Centers for Disease Control and Prevention cooperative agreement number NUE1EH001393. With permission of the MO HealthNet Data Project Committee.